Blog
February 20, 2020
Multifocal motor neuropathy (MMN) is one of many rare diseases that can be treated using intravenous immune globulin (IVIg), a therapy that is manufactured from human plasma. This neuropathy is characterized by progressive muscle weakness and muscle wasting, and without regular IVIg treatments, a patient’s quality of life can decline. In today’s blog, we’ll be unpacking everything you need to know about multifocal motor neuropathy and how plasma donations play a vital role in treating this condition.
What are the Symptoms of Multifocal Motor Neuropathy?
Multifocal motor neuropathy is a disorder that occurs when the body’s motor nerves, the nerves that control muscles, are attacked by one’s own immune system. This makes it difficult for the body to send the electrical signals needed for controlled movement, which can result in the following symptoms occurring:
· Weakness, cramping and/or twitching in the hands and arms.
· Weakness, cramping and/or twitching that is more severe on one side of the body.
· Wrist drop or foot drop.
· Wasting (atrophy) of affected muscles.
Early symptoms typically start in specific parts of a person’s arm or hand, such as their wrist. Muscle atrophy is a symptom that occurs much later on in the course of the condition.
What are the Causes of Multifocal Motor Neuropathy?
The causes of MMN are not fully understood, but scientists have identified this condition as an autoimmune disease that is the result of an abnormal immune system response. Researchers are studying MMN in an effort to better understand the underlying causes of this disease.
How is Multifocal Motor Neuropathy Diagnosed?
Diagnosing a patient with MMN typically requires a physical exam as well as nerve and blood tests that entail the following:
· A needle electromyography that uses electrodes that are placed in a patient’s arm to measure the electrical activity in their muscles.
· A nerve conduction study in which two sensors are put overtop the skin of a nerve and small electric shocks are transmitted to measure how quickly electrical signals can travel through a patient’s nerves.
· A blood test that specifically looks for GM1 antibodies, which is a part of the body’s immune system that some people with MMN have elevated levels of.
· Evidence of a purely motor disorder that affects individual nerves
Doctors sometimes mistake MMN for ALS, also referred to as Lou Gehrig’s disease. To minimize the chance of this happening, they also check to make sure that patients aren’t showing any signs of difficulty speaking or swallowing, there’s no indication of sensory deficits, and that upper motor neuron signs like swift reflexes at the knee aren’t present.
How is Multifocal Motor Neuropathy Diagnosed?
Multifocal motor neuropathy is not a life-threatening disease, but it can slowly worsen over time and make daily tasks more strenuous. Intravenous immune globulin is a treatment manufactured from donated plasma that can improve a patient’s muscle strength.
IVIg is administered to MMN patients through an IV that is given every two to six weeks since the effects of the treatment wear off after a few months. Regular maintenance IVIg infusions typically make day-to-day life much more manageable for those living with MMN.
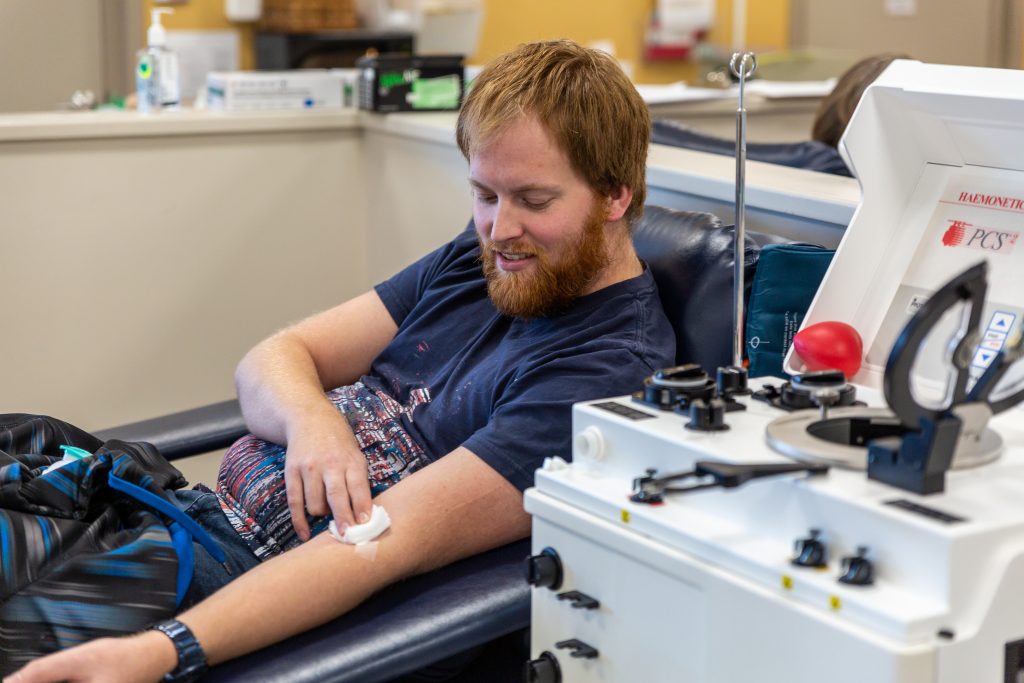
The important role donated plasma plays in treating multifocal motor neuropathy is just one example of what this miracle liquid is capable of and the effect it can have on the lives of individuals that have rare and chronic conditions. That’s why we’ve committed ourselves to collecting plasma that can be manufactured into lifesaving therapies at DB Plasma.
To contribute to a good cause and change the life of patients in need, book your next appointment at a DB Plasma centre near you.