Blog
January 5, 2021

The holiday season is all about the giving spirit. After everything we’ve gone through this past year, the importance of giving back has become more apparent than ever before. If you’re looking for a good cause to contribute to this holiday season, you should consider plasma donation!
Here are three reasons to donate plasma during the season of giving.
1. The Growing Demand for Plasma Donations
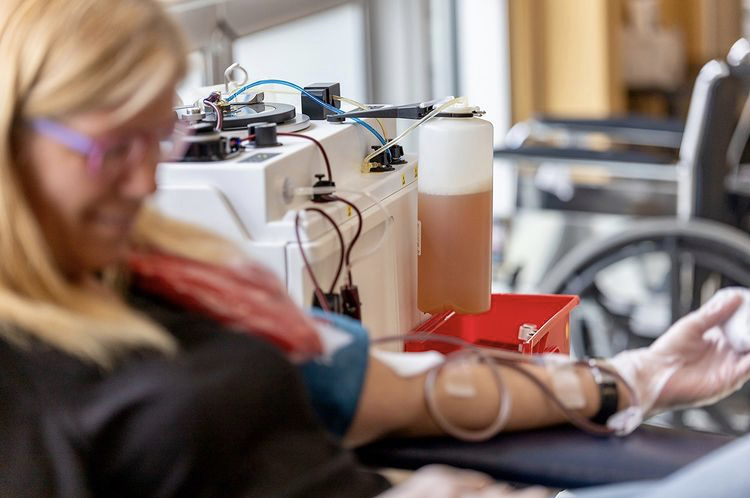
Blood plasma is used to treat several rare conditions, including Primary Immunodeficiency Diseases (PIDs) and Alpha-1 Antitrypsin Deficiency, just to name a few. The demand for this straw-coloured liquid portion of blood is only growing, and Canada is among the leading users of human plasma products in the world. Currently, we rely on paid plasma donations from the US to manufacture the majority of our nation’s plasma therapies.
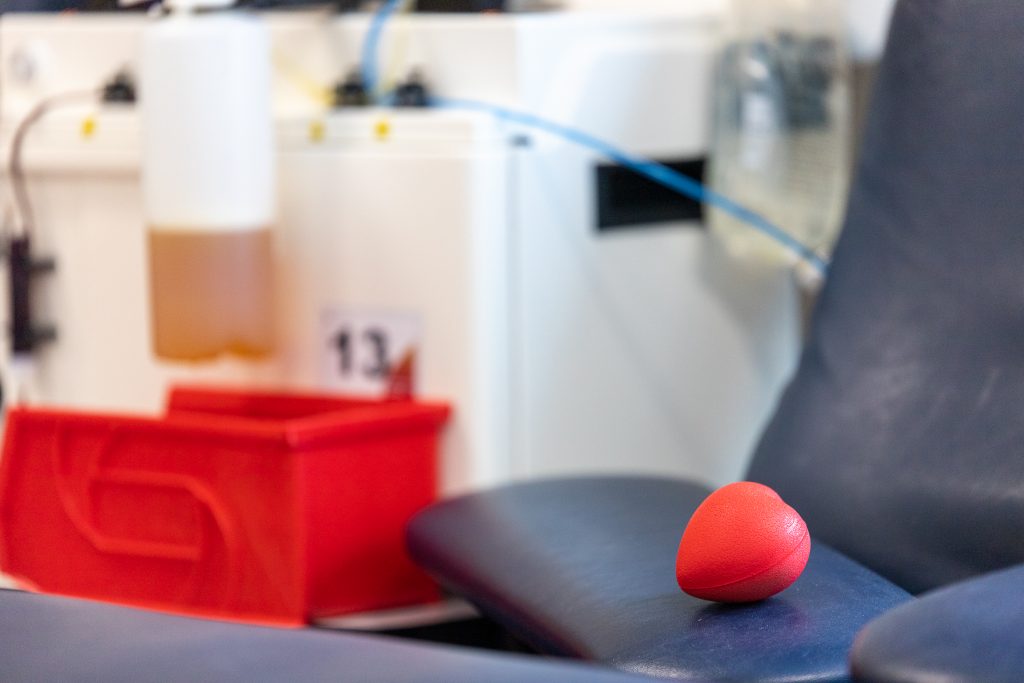
By donating plasma at DB Plasma, you can help pharmaceutical manufacturers meet the growing demand for plasma products. You’ll also have the opportunity to earn up to $400/month for your donations.
2. Contributing to Convalescent Plasma Therapies
Canada began rolling out Pfizer’s COVID-19 vaccine last week, which was a moment we’ve all been waiting for since this pandemic began. While the arrival of the COVID-19 vaccine does signal the beginning of the end, we still have many challenging months ahead of us. Convalescent plasma, the term used for plasma that is collected from an individual who has recovered from a virus, will likely still play a role in helping patients affected by COVID-19.
Since May, DB Plasma has been accepting convalescent plasma donations from COVID-19 survivors and testing all plasma donations for antibodies to SARS-CoV-2. Your plasma donations can help find a potential treatment for COVID-19.
3. Donating Plasma Is A Great Way to Give Back
Patients with immune deficiencies and autoimmune diseases rely on the generosity of others to access the treatments they need. Remaining in good health is especially important for these patients during these uncertain times.
DB Plasma is the largest producer of normal and specialty human source plasma for further manufacturing in Canada. When you donate plasma at our centres, you can rest assured that your donations will be making a big difference in the lives of immunocompromised patients.
Plasma donation truly encompasses the spirit of the holidays. To help patients in need during the holiday season and get compensated for your contribution, book an appointment at a DB Plasma centre near you!